Understanding the Impact of Modern Heart Medications
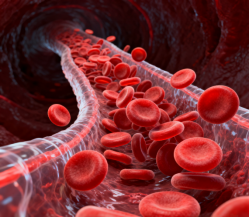
The battle against heart disease continues to evolve with breakthrough developments in cardiovascular drugs. These powerful medications have transformed the landscape of cardiac care, offering hope and healing to millions worldwide. As heart disease remains a leading cause of mortality globally, the role of cardiovascular drugs has become increasingly crucial in both prevention and treatment strategies. Modern pharmaceutical innovations have created a robust arsenal of medications that target various aspects of heart health, from blood pressure management to cholesterol control.
The effectiveness of cardiovascular drugs extends beyond simply treating symptoms – they work at multiple levels to protect heart function, strengthen cardiac tissue, and prevent potentially life-threatening complications. Medical professionals now have access to sophisticated treatment options that can be tailored to individual patient needs, marking a significant advancement in personalized cardiac care.
The Science Behind Cardiovascular Drug Action
Mechanism of Action in Heart Protection
Cardiovascular drugs operate through diverse biochemical pathways to safeguard heart health. Beta-blockers, for instance, work by blocking the effects of stress hormones on the heart, effectively reducing heart rate and blood pressure. ACE inhibitors dilate blood vessels, making it easier for the heart to pump blood throughout the body. Understanding these mechanisms helps healthcare providers select the most appropriate medications for specific cardiac conditions.
The sophisticated design of modern cardiovascular drugs allows for targeted intervention at various points in the cardiovascular system. Some medications focus on preventing blood clot formation, while others work to strengthen heart muscle contractions or regulate heart rhythm. This multi-faceted approach ensures comprehensive protection against heart disease progression.
Timing and Duration of Drug Effects
The timing of cardiovascular drug administration plays a crucial role in their effectiveness. Some medications provide immediate relief from acute symptoms, while others build protective effects over time through consistent use. Long-acting formulations have revolutionized treatment protocols, allowing for better compliance and more stable drug levels in the bloodstream.
Maintaining appropriate drug concentrations in the body requires careful consideration of factors such as metabolism, elimination rates, and potential drug interactions. Healthcare providers carefully monitor these aspects to optimize treatment outcomes while minimizing side effects.
Categories of Heart Disease Prevention Medications
Primary Prevention Strategies
Primary prevention medications focus on reducing the risk of initial cardiovascular events in individuals with risk factors but no established heart disease. Statins represent a cornerstone of primary prevention, effectively lowering cholesterol levels and reducing the likelihood of heart attacks and strokes. These cardiovascular drugs have demonstrated remarkable success in preventing the onset of serious cardiac conditions.
Blood pressure medications also play a vital role in primary prevention, helping maintain optimal circulatory function and reducing stress on the heart. The combination of different drug classes often provides synergistic benefits, enhancing overall protective effects.
Secondary Prevention Protocols
For individuals who have already experienced cardiac events, secondary prevention becomes crucial. This approach typically involves more intensive medication regimens, combining multiple cardiovascular drugs to prevent further complications. Antiplatelet agents, such as aspirin and newer P2Y12 inhibitors, help prevent dangerous blood clots from forming.
The management of established heart disease often requires a comprehensive medication strategy that addresses multiple risk factors simultaneously. This might include combinations of antihypertensives, lipid-lowering agents, and medications to control heart rhythm or strengthen heart contractions.
Optimizing Treatment Outcomes
Personalized Medicine Approaches
The future of cardiovascular drug therapy lies in personalization. Genetic testing and biomarker analysis help identify which medications will work best for individual patients. This targeted approach improves treatment efficiency while reducing the risk of adverse effects. Healthcare providers can now make more informed decisions about medication selection and dosing based on patient-specific factors.
Advanced diagnostic tools enable continuous monitoring of treatment effectiveness, allowing for real-time adjustments to medication regimens. This dynamic approach to cardiovascular drug management ensures optimal outcomes for each patient.
Lifestyle Integration and Medication Management
The success of cardiovascular drugs depends heavily on their integration with healthy lifestyle practices. Regular exercise, proper diet, and stress management complement medication effects, creating a comprehensive approach to heart disease prevention. Patient education about the importance of medication adherence and lifestyle modifications plays a crucial role in treatment success.
Healthcare providers work closely with patients to develop sustainable routines that incorporate both medication schedules and healthy habits. This collaborative approach improves long-term outcomes and reduces the risk of treatment failure.
Future Developments in Cardiac Medicine
Emerging Drug Technologies
Research continues to unveil promising new cardiovascular drugs and delivery systems. Novel molecular targets are being identified, leading to the development of more selective and effective medications. These innovations promise to further improve the precision and effectiveness of heart disease treatment.
Advanced drug delivery systems, including long-acting formulations and targeted release mechanisms, are revolutionizing how cardiovascular drugs are administered. These developments aim to enhance patient compliance while maximizing therapeutic benefits.
Integration with Digital Health Solutions
The integration of cardiovascular drug therapy with digital health technologies is creating new opportunities for treatment optimization. Smart devices and mobile applications help track medication adherence, monitor vital signs, and provide real-time feedback to healthcare providers. This technological integration improves treatment outcomes while enabling early detection of potential problems.
Artificial intelligence and machine learning algorithms are being developed to predict patient responses to different cardiovascular drugs, further advancing the field of personalized medicine.
Frequently Asked Questions
How long does it take for cardiovascular drugs to show effects?
The timeframe for cardiovascular drugs to demonstrate effects varies depending on the type of medication and the condition being treated. Some medications, like nitroglycerin for angina, work within minutes, while others, such as statins, may take several weeks to show significant benefits. Consistent use according to prescribed schedules is essential for optimal results.
Can cardiovascular drugs be taken with other medications?
While many cardiovascular drugs can be safely combined with other medications, it's crucial to inform your healthcare provider about all medications you're taking, including over-the-counter drugs and supplements. Some combinations may interact and require dosage adjustments or alternative treatments to ensure safety and effectiveness.
What lifestyle changes should accompany cardiovascular drug therapy?
To maximize the benefits of cardiovascular drugs, patients should maintain a heart-healthy lifestyle that includes regular physical activity, a balanced diet low in saturated fats and sodium, stress management, and smoking cessation if applicable. These lifestyle modifications work synergistically with medications to improve overall cardiovascular health and treatment outcomes.